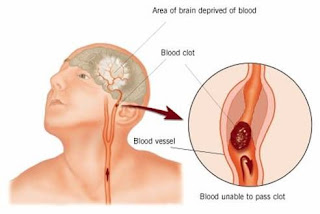
The symptoms of a cerebral vascular accident depend on which part of the brain is affected. Common symptoms may include paralysis of a part of the body, loss of all or part of the vision, or loss of the ability to speak or to understand speech.
A stroke is a medical emergency and can cause permanent neurological damage, complications, and death. Risk factors for stroke include old age, high blood pressure, previous stroke or transient ischemic attack (TIA), diabetes, high cholesterol, tobacco smoking and atrial fibrillation. High blood pressure is the most important modifiable risk factor of stroke. It is the second leading cause of death worldwide.
Stroke symptoms typically start suddenly, over seconds to minutes, and in most cases do not progress further. The symptoms depend on the area of the brain affected. The more extensive the area of brain affected, the more functions that are likely to be lost. Some forms of stroke can cause additional symptoms. For example, in intracranial hemorrhage, the affected area may compress other structures. Most forms of stroke are not associated with headache, apart from subarachnoid hemorrhage and cerebral venous thrombosis and occasionally intracerebral hemorrhage.
Stroke is diagnosed through several techniques: a neurological examination (such as the Nihss), CT scans (most often without contrast enhancements) or MRI scans, Doppler ultrasound, and arteriography. The diagnosis of stroke itself is clinical, with assistance from the imaging techniques. Imaging techniques also assist in determining the subtypes and cause of stroke. There is yet no commonly used blood test for the stroke diagnosis itself, though blood tests may be of help in finding out the likely cause of stroke.
Nursing Diagnosis for CVA - Stroke:
1. Ineffective Cerebral Tissue Perfusion
2. Impaired Physical Mobility.
3. Imbalanced Nutrition, Less Than Body Requirements.
4. Impaired Skin Integrity.
5. Impaired Verbal Communication
6. Disturbed Sensory Perception
7. Self-Care Deficit
8. Knowledge Deficit